Make An Appointment
Simplifying Surgery Experience
Consult with our expert surgeon for more than 50+ diseases
- Once you share your details, our care coordinator will get in touch with you.
- The coordinator will understand your symptoms and health condition in detail.
- Your consultation will be scheduled at the earliest.
ACL Tear Surgery - Treatment Procedure & Benefits at Curific Health Care
Get In Touch
Make an Appointment
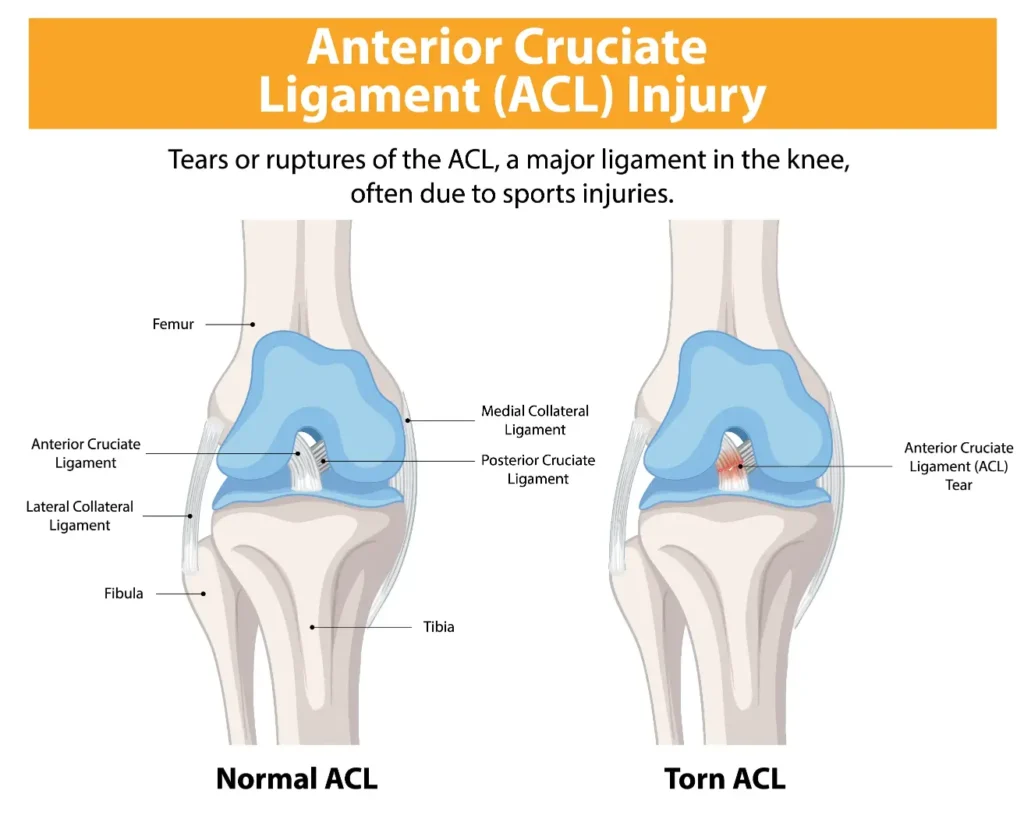
What is ACL Tear?
An anterior cruciate ligament (ACL) injury refers to a tear or sprain of the ACL, which is located on the inside of the knee joint. The ACL plays a key role in stabilizing the knee by connecting the thigh bone to the shin bone. ACL injuries are most common in athletes who engage in high-impact sports such as football, basketball, and soccer. The injury often occurs during activities that involve sudden stops, jumps, or changes in direction.
In many cases, individuals may hear a popping sound or feel a popping sensation at the time of the injury.
Treatment for ACL Tear
The treatment for an ACL tear depends on the severity of the injury:
Severe ACL Tears: In cases where the ACL is significantly torn, surgery is usually required to restore stability to the knee. Without surgery, the knee may remain unstable, leading to further damage and chronic pain.
Mild ACL Tears: For minor ACL injuries, non-surgical treatments such as rest, physical therapy, and rehabilitation exercises can help improve strength, flexibility, and stability of the knee. Rest and avoiding activities that exacerbate the injury are essential for recovery.
For both severe and mild injuries, prompt treatment is essential to prevent long-term complications, such as chronic pain or the development of osteoarthritis in the knee.
Make An Appointment
Simplifying Surgery Experience
Consult with our expert surgeon for more than 50+ diseases
- Once you share your details, our care coordinator will get in touch with you.
- The coordinator will understand your symptoms and health condition in detail.
- Your consultation will be scheduled at the earliest.
How is an ACL Injury Diagnosed?
The diagnosis of an ACL injury typically begins with a physical examination by a healthcare provider. The doctor will check for swelling, tenderness, and range of motion in the knee, as well as assess its overall function. The knee may be moved into various positions to evaluate its stability and detect any signs of instability, which is common in ACL tears.
To confirm the diagnosis and determine the severity of the injury, the doctor may recommend imaging tests, such as:
X-rays: X-rays are used to rule out any bone fractures, as they cannot detect soft tissue injuries like ligament tears.
Magnetic Resonance Imaging (MRI): An MRI uses radio waves and a magnetic field to produce detailed images of both hard and soft tissues, including ligaments, tendons, and cartilage. This test can show the extent of the ACL injury and any damage to surrounding tissues.
Ultrasound: This imaging technique uses sound waves to visualize internal structures, such as ligaments, tendons, and muscles, to detect any tears or injuries.
These diagnostic tests help doctors determine the exact nature and severity of the ACL injury, allowing them to recommend the most appropriate treatment plan.
Get In Touch
Make an Appointment
Make An Appointment
Simplifying Surgery Experience
Consult with our expert surgeon for more than 50+ diseases
- Once you share your details, our care coordinator will get in touch with you.
- The coordinator will understand your symptoms and health condition in detail.
- Your consultation will be scheduled at the earliest.
What are the Different ACL Reconstruction Treatment Options?
There are both surgical and non-surgical treatment options available for ACL reconstruction, depending on the severity of the injury and the patient’s condition.
Surgical Treatment Options:
Knee Arthroscopy:
Knee arthroscopy is a minimally invasive surgery where a thin tube with a camera is inserted through small incisions in the knee to visualize the joint. This allows the surgeon to assess the extent of the injury and repair the torn ACL. The surgeon may also remove damaged bone, cartilage, or inflamed tissue. The incision is then closed with stitches, and the knee is wrapped with a bandage. This procedure is often preferred due to its smaller incisions and quicker recovery time.Knee Ligament Repair:
This outpatient procedure involves replacing the damaged ligament with a healthy tendon from another part of the body or a donor. The surgery is performed under anesthesia, and the recovery time is relatively short. This treatment option is generally recommended for patients with less severe injuries or those who need a quicker recovery.
Non-Surgical Treatment Options:
For those with minor ACL injuries or patients who may not require immediate surgery, non-surgical treatments can help manage symptoms and promote healing:
Ice Therapy:
Applying ice to the knee several times a day can help reduce swelling and pain.Elevation:
Elevating the knee above the level of the heart can help decrease swelling and improve circulation.Rest:
Reducing or stopping physical activity for a few weeks can give the knee time to heal and reduce strain on the injured ACL.Compression:
Using a bandage or wrap to compress the knee can help control swelling and stabilize the knee joint.Anti-inflammatory Medications:
Over-the-counter anti-inflammatory drugs like ibuprofen can help alleviate pain and swelling, speeding up the recovery process.
The appropriate treatment for an ACL injury depends on various factors, including the severity of the tear, the patient’s activity level, and their overall health. Your doctor will guide you through the best treatment plan based on your specific condition.
Benefits of Arthroscopic ACL Reconstruction Surgery
Arthroscopic ACL reconstruction surgery offers several significant benefits, making it a preferred treatment option for those with severe ACL injuries:
Restoration of Knee Function:
ACL tears can severely impact the knee’s functionality, making it difficult to perform everyday activities. Arthroscopic ACL reconstruction surgery is the most effective method to restore knee stability and function. By permanently repairing the torn ACL, the surgery addresses the root cause of the issue, allowing patients to return to their normal activities and regain full mobility.Significant Symptom Relief:
ACL tears often cause pain, swelling, weakness, and reduced functionality in the knee. Non-surgical treatments can provide temporary relief, but they do not heal the torn ligament. Arthroscopic surgery significantly reduces pain, swelling, and the limitations caused by an ACL injury, offering long-term relief.Prevention of Further Damage:
An untreated ACL tear can lead to further damage to the knee’s cartilage and surrounding structures. By stabilizing the knee, ACL reconstruction surgery helps prevent additional strain and injuries to the joint, preserving the long-term health of the knee.Cost-Effective:
Compared to prolonged physical therapy, bracing, or other non-surgical treatments, arthroscopic ACL surgery is often more cost-effective in the long run. It addresses the problem directly, reducing the need for ongoing treatments and minimizing recovery time.
Overall, arthroscopic ACL reconstruction is a highly effective, minimally invasive procedure that helps restore knee function, relieve symptoms, prevent further damage, and offer long-term, cost-effective benefits.
Make An Appointment
Simplifying Surgery Experience
Consult with our expert surgeon for more than 50+ diseases
- Once you share your details, our care coordinator will get in touch with you.
- The coordinator will understand your symptoms and health condition in detail.
- Your consultation will be scheduled at the earliest.
Timeline For ACL Surgery Recovery
The recovery timeline after anterior cruciate ligament (ACL) reconstruction surgery can vary based on several factors, including the patient’s fitness level, the type of surgery, and the post-operative care provided. Here is a general recovery timeline:
Weeks 1-3
The first three weeks are crucial for healing. Focus on proper nutrition and ice application to control inflammation. Early rehabilitation includes strengthening the leg muscles, particularly the quadriceps (thigh muscles), which are essential for walking, stair climbing, and standing up from a seated position. Improving knee mobility is also important to aid healing and enhance function.
Weeks 4-6
During this phase, tendon remodeling occurs if a graft from the patient’s own tendon is used. The tendon breaks down and transforms into ligament tissue to handle the forces required by the ACL. By the end of this period, many patients are able to walk without assistive devices or a brace, assuming adequate muscle strength and knee mobility. Bending the knee to perform tasks like putting on pants becomes easier.
Weeks 6-12
The knee can tolerate greater loads, and patients notice significant improvements in strength and function. Rehabilitation focuses on activity-specific exercises, such as squats, stair climbing, and balancing. Biking with resistance is also introduced. This period is crucial for building strength, endurance, and control to prepare for more strenuous activities, including those needed for sports or work.
3-6 Months
By this time, the ACL graft has gained strength, and patients can begin impact activities like running and jumping. Muscular control and stability continue to improve, but exercises must be performed with proper form to avoid excess strain on the reconstructed ACL. Training for proper jumping, landing, and cutting techniques is important to prevent re-injury, as improper form during these activities can strain the ACL.
6-12 Months
At this stage, patients often feel better and can resume more physical activities like squatting, jumping, and running. Contact sports can typically be resumed after 6 months, but full recovery may take up to 12 months. During this time, it’s essential to monitor lower extremity alignment and control during high-impact activities to reduce the risk of re-injury. Careful attention to form while cutting, jumping, and running is necessary for complete recovery.
Each recovery phase is vital for restoring full knee function, and patients should follow their rehabilitation plan diligently to ensure the best possible outcome.
Risk and Complications of ACL Surgery
Like any surgical procedure, ACL surgery also carries certain risks and complications, including
- Anterior knee pain: The most common complication after ACL surgery is pain around the kneecap. It usually occurs in the patient who has surgery performed with a patellar tendon graft, as this procedure involves the removal of bone from the kneecap.
- Stiffness (arthrofibrosis): It is quite common to experience stiffness in the knee joint after an ACL injury. However, in most cases, it can be easily managed with aggressive rehabilitation. In some rare instances, a ball of scar tissue forms in the front of the knee, even despite rehabilitation. It can also lead to an inability to straighten the knee fully.
- Instability: In some cases, after reconstruction surgery, instability of the knee occurs. It is the result of a surgical error or an undiscovered injury that occurred in or around the knee at the time of ACL tear.
- Graft stretching: When an ACL is reconstructed, the ACL is replaced by an autograft or allograft. In autograft, bone or tissue is transferred from one part of a patient’s body to another. An allograft is a transfer of bone or tissue from a donor or cadaver. In some cases, the graft used to replace a torn ACL is stretched, potentially leading to other complications like instability or graft failure.
- Ganglion cyst formation: A rare complication from ACL reconstruction surgery is the formation of a cyst within or around the graft. These cysts are usually harmless and can be routinely removed, but they can sometimes cause symptoms like Knee pain, clicking of the knee, reduced knee extension, and stiffness.
- Growth plate injury: Bleeding at the incision site of an ACL surgery is common but can be a concern if the blood is excessive enough that it soaks through wound dressings and does not stop after pressure is applied to the area.
- Bleeding: Bleeding at the incision site of an ACL surgery is common but can be a concern if the blood is excessive enough that it soaks through wound dressings and does not stop after pressure is applied to the area. The reason for bleeding after ACL surgery varies and is usually caused by an underlying issue. For example, in some cases, injury to an artery during surgery may cause bleeding, and surgically repairing the artery will stop the bleeding from continuing.
- Disease transmission: Infection is a rare complication but can be serious when it occurs. When the infection is inside the knee joint, there is a concern about the ACL graft becoming infected. If the infection is serious and does not get better with antibiotics, the graft may need to be surgically cleaned or removed to eliminate the infection.
- Blood clots: Following ACL surgery, blood clots can form in the thigh or calf, with the potential to break off in the bloodstream and travel to other parts of the body, such as the lungs or brain.The reason for blood clots that develop after ACL surgery is unknown, but research suggests that factors can include a personal history of blood clotting, age (over 30 years), and hypertension.
- Re-Rupture of the ACL Graft: Repeat rupture of the ACL graft is uncommon but sometimes occurs. Whenever there is a re-rupture of the graft, a surgeon should carefully assess for possible technical failures of the first surgery. Possible problems that can lead to the re-tear of the ACL include suboptimal positioning of the graft, improper tension on the graft, or failure of the fixation of the graft.
Rehabilitation for ACL Injury for Athletes
Rehabilitation after ACL surgery for athletes is typically longer than for non-athletes due to the increased strain on the joints during sports activities. The goal of the rehabilitation process is to restore function, prevent re-injury, and prepare the athlete to safely return to their sport. The rehabilitation is usually structured in the following phases:
Phase 1: 3-4 Months Post-Surgery
- Goal: Regain strength and improve joint flexibility.
- Focus on reducing swelling and pain, improving the range of motion, and strengthening the quadriceps and hamstring muscles.
- Gentle range of motion exercises and basic strengthening exercises are introduced.
- Early rehabilitation may include low-impact exercises like stationary biking and leg lifts.
Phase 2: 4-6 Months Post-Surgery
- Goal: Build low-level fitness and start performance agility drills.
- Athletes begin working on more intense strengthening exercises and low-impact agility drills like ladder drills, short sprints, and bodyweight exercises.
- The focus is on regaining strength, improving stability, and starting to integrate more dynamic movements to mimic sports activities.
- This phase helps to prepare the body for more explosive movements in later stages.
Phase 3: 5-8 Months Post-Surgery
- Goal: Introduce jumping exercises.
- Jumping drills are incorporated into the rehabilitation process to regain function and flexibility in the knee joint.
- This phase also focuses on restoring neuromuscular control, balance, and coordination to avoid improper landing mechanics.
- Exercises may include jumping over small hurdles, plyometric exercises, and controlled vertical jumps.
Phase 4: 6-9 Months Post-Surgery
- Goal: Introduce single-leg jumping exercises and sports-specific cutting drills.
- Athletes begin more complex exercises, such as single-leg hopping and cutting (sharp changes in direction) drills.
- Agility and coordination are improved to prepare the athlete for the dynamic movements required in their sport.
- Emphasis is placed on proper mechanics during cutting, pivoting, and deceleration to prevent re-injury.
Phase 5: 9-12 Months Post-Surgery
- Goal: Steadily increase sports drills to match prior skill levels and prevent re-injury.
- Athletes begin sport-specific drills at full intensity, including high-impact movements like running, cutting, and jumping.
- Drills mimic the demands of the athlete’s sport, such as directional changes, sprints, and agility training.
- The athlete’s technique and strength are closely monitored to ensure that the knee is stable, and proper form is maintained to minimize the risk of re-injury.
Throughout the entire rehabilitation process, athletes are encouraged to focus on flexibility, strength, stability, and proper technique. They should also be diligent in avoiding early returns to full activity, as rushing back too soon can increase the risk of re-injury. Complete rehabilitation is essential to ensuring a successful return to sports and a reduced risk of further ACL injuries.
Make An Appointment
Simplifying Surgery Experience
Consult with our expert surgeon for more than 50+ diseases
- Once you share your details, our care coordinator will get in touch with you.
- The coordinator will understand your symptoms and health condition in detail.
- Your consultation will be scheduled at the earliest.
Types of ACL Surgery Grafts
There are several types of grafts used in ACL reconstruction surgery, each chosen based on the patient’s needs, activity level, and the surgeon’s recommendation. The three primary types of grafts are:
1. Patellar Tendon Autograft
- Description: This graft involves harvesting the central one-third of the patellar tendon, which connects the kneecap (patella) to the tibia (shinbone). A small piece of bone is also taken from both the patella and tibia to create a bone-tendon-bone graft.
- Advantages:
- Provides a strong initial fixation.
- The tendon regenerates in the donor knee over time.
- It is one of the most commonly used grafts due to its strong attachment and durability.
- Disadvantages:
- Can cause more pain at the donor site (patellar tendon).
- Slightly higher risk of developing patellofemoral pain (pain in the front of the knee).
2. Hamstring Autograft
- Description: This graft is taken from the tendons of the hamstring muscles at the back of the thigh. Typically, two tendons are harvested from the leg undergoing ACL reconstruction, and they are bundled together to form a tissue graft.
- Advantages:
- Smaller incision required for harvesting the tendon.
- Lower risk of developing patellofemoral pain compared to the patellar tendon graft.
- A strong graft that is less likely to cause pain at the donor site.
- Disadvantages:
- The fixation strength is not as strong as the bone-to-bone fixation of the patellar tendon graft, but improvements in fixation techniques continue to be made.
- The hamstring tendon regenerates, but may not be as strong as the original tissue.
3. Allograft
- Description: This graft is taken from a cadaver donor. It is commonly used when the patient prefers not to have a second surgical site for harvesting a tendon.
- Advantages:
- No need for an additional incision to harvest tissue, making it less invasive.
- Decreased operative time and less post-operative pain.
- Suitable for non-competitive athletes or older individuals who do not require the highest level of athletic performance.
- Disadvantages:
- Not as strong as a patient’s own tissue, which may be a concern for highly active or younger athletes.
- There is a very small risk of disease transmission, though screening and sterilization techniques significantly reduce this risk.
- Minimal risk of graft rejection, as the tissue is thoroughly processed.
Each graft type has its own set of advantages and considerations, and the choice is made based on factors like the patient’s age, activity level, and whether they want to avoid additional incisions. The surgeon will discuss the best option based on the individual’s needs and recovery goals.