Make An Appointment
Simplifying Surgery Experience
Consult with our expert surgeon for more than 50+ diseases
- Once you share your details, our care coordinator will get in touch with you.
- The coordinator will understand your symptoms and health condition in detail.
- Your consultation will be scheduled at the earliest.
Balanitis Treatment - Surgery Procedure & Operation Benefits at Curific Health Care
Get In Touch
Make an Appointment
What is Balanitis Infection?
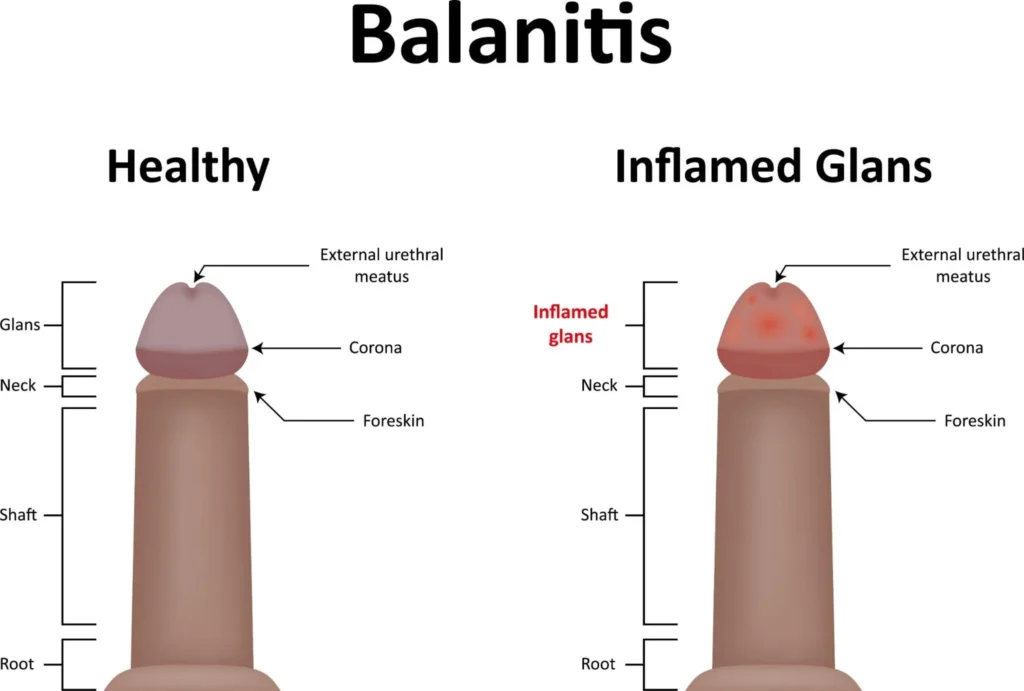
Balanitis is a condition characterized by pain, inflammation, and irritation of the glans (head) of the penis, often caused by an infection in the skin. While yeast infections, particularly candida balanitis, are among the most common causes, balanitis can also result from bacterial infections, poor hygiene, or allergic reactions.
Causes of Balanitis:
- Yeast Infections (Candida Balanitis): This is one of the most frequent causes of balanitis. It is often triggered by an overgrowth of yeast (Candida) in the genital area.
- Bacterial Infections: Infections caused by bacteria can also lead to balanitis. These can be due to poor hygiene or other underlying health conditions.
- Improper Hygiene: Inadequate cleaning of the genital area, especially in uncircumcised men, can lead to a buildup of bacteria or fungi, increasing the risk of balanitis.
- Allergic Reactions: Sensitivity or allergic reactions to latex condoms or certain medications can also cause balanitis.
- Sexually Transmitted Diseases (STDs): Some STDs, such as gonorrhea or chlamydia, can cause balanitis as a symptom.
Symptoms of Balanitis:
- Rashes on the Penis: Red, purple, gray, or white rashes, along with itching or irritation on the glans, are common signs of balanitis.
- Red Spots on the Penis: These can appear on the glans and are typically associated with balanitis.
- Balanitis Bumps: In rare cases, balanitis may lead to the development of scaly warts or bumps, a condition known as Pseudoepitheliomatous Keratotic and Micaceous Balanitis (PKMB).
- Redness on Foreskin: Along with the glans, the foreskin may also show signs of inflammation, including redness or itchiness.
Treatment Options:
Balanitis is typically not a serious condition and can often be treated effectively with antifungal creams or antibiotics, depending on the underlying cause. However, if these treatments are ineffective, urologists may recommend circumcision as a more permanent solution, especially if the infection persists or recurs frequently.
Contagion:
While balanitis itself is not contagious, the underlying infection causing the condition—such as a yeast infection or STD—can be transmitted to others. It’s important to seek treatment to prevent the spread of the infection.
Conclusion:
Balanitis is a treatable condition, though it can be painful and uncomfortable. If symptoms like rashes, redness, or irritation persist, it’s important to seek medical advice to determine the underlying cause and appropriate treatment.
Common Types of Balanitis
Balanitis is categorized into different types based on the causes and symptoms. Here are the three most common types of balanitis:
-
Zoon’s Balanitis
Zoon’s Balanitis, also known as plasma cell balanitis, is the most prevalent form of balanitis. It typically affects uncircumcised men, especially those who are middle-aged or older. This condition causes the tip of the penis to become inflamed and appear red. The initial treatment usually involves maintaining proper hygiene and applying emollient creams to soothe the area. If the condition persists, circumcision is often considered a curative treatment. -
Circinate Balanitis
Circinate Balanitis is a type of balanitis associated with reactive arthritis, a form of arthritis triggered by an infection elsewhere in the body. In addition to redness and inflammation of the glans, this type of balanitis causes small lesions or sores on the penis. Initially, it presents as small dots with a white plaque, which later develop into red patches with no white borders. One of the distinguishing features of Circinate Balanitis is that it does not cause itching, burning sensations, or unpleasant odors. -
Pseudoepitheliomatous Keratotic and Micaceous Balanitis (PKMB)
PKMB is a rare form of balanitis that primarily affects men over the age of 60. It is characterized by the development of warts on the glans of the penis. Although PKMB is often asymptomatic, it can sometimes lead to maceration (softening of the skin), fissuring, and irritation. This condition has a chronic course and can recur even after treatment. Treatment typically focuses on managing the symptoms and preventing recurrence.
Conclusion
Each type of balanitis has its own set of symptoms and treatment options. While most cases can be treated with proper hygiene and topical medications, more severe or persistent cases may require surgical interventions like circumcision. If you experience any symptoms of balanitis, it is important to consult a healthcare provider for proper diagnosis and treatment.
Make An Appointment
Simplifying Surgery Experience
Consult with our expert surgeon for more than 50+ diseases
- Once you share your details, our care coordinator will get in touch with you.
- The coordinator will understand your symptoms and health condition in detail.
- Your consultation will be scheduled at the earliest.
Causes of Balanitis
Balanitis is more commonly seen in uncircumcised men compared to circumcised ones. The primary cause of balanitis is poor hygiene practices. When hygiene is not properly maintained, microbes such as bacteria, fungi, and yeast can thrive in the warm, moist area beneath the foreskin, leading to infections. These infections can result in swelling of the head of the penis and sometimes the foreskin. Some other causes of balanitis include:
-
Infection (Non-Sexually Transmitted)
A common cause of balanitis is a yeast or bacterial infection. The fungus Candida is often the culprit behind these infections. Various germs present on the skin can multiply and cause an infection, leading to inflammation and discomfort in the affected area. -
Infection (Sexually Transmitted)
Although less common, some sexually transmitted infections (STIs) can also lead to balanitis. This typically occurs when there is swelling of the urethra, and it may be associated with other symptoms like pain or discharge. STIs that cause balanitis include gonorrhea, chlamydia, and herpes. -
Skin Conditions
Certain skin conditions can also contribute to the development of balanitis. Psoriasis is one of the common skin conditions that can affect the penis and lead to inflammation of the glans. Other skin conditions, such as eczema, lichen planus, and lichen sclerosus, can also cause balanitis but are less frequently linked. -
Allergic Irritants
The skin on the penis is sensitive and can become irritated by certain products or chemicals. Some common allergens and irritants include:- Soaps and disinfectants
- Over-washing or scrubbing
- Latex condoms and lubricants
- Certain washing powders or fabric softeners
-
Poor Hygiene
Improper hygiene, especially when accompanied by a tight foreskin, can lead to irritation caused by smegma. Smegma is a whitish, cheesy substance that accumulates under the foreskin if the glans is not cleaned regularly. The buildup of smegma can lead to infections, inflammation, and discomfort.
Conclusion
Maintaining proper hygiene and avoiding irritants or infections are key to preventing balanitis. If you experience symptoms such as redness, irritation, or pain, it is important to consult a healthcare provider for an accurate diagnosis and appropriate treatment.
Get In Touch
Make an Appointment
Make An Appointment
Simplifying Surgery Experience
Consult with our expert surgeon for more than 50+ diseases
- Once you share your details, our care coordinator will get in touch with you.
- The coordinator will understand your symptoms and health condition in detail.
- Your consultation will be scheduled at the earliest.
Diagnosis and Treatment of Balanitis
Diagnosis of Balanitis Infection
Before treating balanitis, your doctor will perform several tests to assess your overall health and identify any underlying medical conditions that may require additional care. A physical examination is typically sufficient to diagnose balanitis, as most of its symptoms are visible. However, your urologist may recommend additional tests to determine the cause and type of balanitis you have:
-
Swab Test
A swab test is commonly used to check for sexually transmitted infections (STIs) or other infections. The doctor will take a sample from the site of infection to analyze it for any pathogens. -
Urinalysis
A urinalysis examines your urine to check for signs of infection or diabetes. It involves analyzing the chemical, visual, and microscopic aspects of your urine. -
Blood Test
A blood test may be done to check for underlying conditions, such as diabetes, or signs of other infections that could be contributing to the balanitis. -
Tissue Biopsy
In some cases, a tissue biopsy may be performed to get a better understanding of the condition. A small sample of cells is taken from the affected area and examined under a microscope to identify the cause of the infection.
Treatment of Balanitis
The treatment for balanitis depends on the underlying cause:
-
Yeast Infection
If the balanitis is caused by a yeast infection (such as Candida), your doctor will recommend antifungal creams to treat the infection. -
Bacterial Infection
If the balanitis is due to a bacterial infection, an antibiotic cream will be prescribed, and proper hygiene should be maintained. In some cases, oral antibiotics may also be required. -
Hygiene Practices
Keeping the affected area clean and dry is essential for recovery, especially when the skin is swollen but not infected. Avoid using soaps, lotions, or chemicals that can irritate the condition. -
Circumcision
For uncircumcised men, circumcision is often the most effective treatment, especially if the balanitis is recurrent. Circumcision involves the removal of the foreskin, which helps prevent the accumulation of urine and other residual matter that can lead to infections. This is especially beneficial for men with a tight, difficult-to-retract foreskin. Stapler circumcision is a modern, minimally invasive method that provides a permanent solution to balanitis by eliminating the risk of recurrent infections.
Balanitis can cause significant discomfort and impact various aspects of life, including sexual health and daily activities. Timely diagnosis and treatment can help alleviate symptoms and prevent further complications.
Make An Appointment
Simplifying Surgery Experience
Consult with our expert surgeon for more than 50+ diseases
- Once you share your details, our care coordinator will get in touch with you.
- The coordinator will understand your symptoms and health condition in detail.
- Your consultation will be scheduled at the earliest.
Surgical Methods of Balanitis Treatment
Circumcision is often considered a safe and effective treatment for balanitis, especially in cases where the infection is recurrent or caused by a tight foreskin. The procedure involves the removal of the foreskin covering the head of the penis. There are three primary methods of performing circumcision:
Laser Circumcision
Laser circumcision is a modern and minimally invasive procedure that uses a high-energy laser beam to remove the foreskin. This method offers several advantages:
- Precision: The laser allows for extremely precise tissue removal with minimal risk of deep cuts or excessive bleeding.
- Shorter Recovery: The recovery period for laser circumcision is typically faster compared to other methods, with better postoperative outcomes.
- Less Pain: Patients usually experience less pain and discomfort during and after the procedure, contributing to a quicker healing process.
Laser circumcision has become a popular option due to its efficiency and the enhanced quality of life after surgery.
Stapler Circumcision
Stapler circumcision is a more conventional and widely used method that is quick, safe, and effective. It involves the use of a specialized, disposable stapler device designed to remove the foreskin. Key features of stapler circumcision include:
- Quick and Efficient: The device works quickly to remove the foreskin in one motion, reducing surgery time.
- Minimal Bleeding: The stapler device also leaves behind a silicone ring that helps close the wound and reduce bleeding.
- Self-Removal: After the wound heals, the silicone ring naturally falls off within 7-10 days, making it a convenient method with minimal post-surgical care.
Stapler circumcision is popular due to its simplicity and faster recovery time compared to traditional methods.
Open Circumcision
Open circumcision, also known as the dorsal slit technique, is a traditional method where the foreskin is removed using a scalpel or surgical scissors. During the procedure:
- Incision: The surgeon makes a cut along the upper length of the foreskin to expose the head of the penis.
- Longer Recovery: Open circumcision is more invasive than laser or stapler circumcision and typically requires a longer healing time.
- Higher Risk of Complications: Due to its invasiveness, this method carries a higher risk of complications during and after surgery, such as infection, excessive bleeding, and scarring.
While effective, open circumcision is less commonly used today because of its longer recovery time and greater risks compared to more modern techniques.
Each of these surgical methods has its advantages, and the choice of procedure depends on the patient’s specific condition, the surgeon’s recommendation, and the desired outcomes.
Make An Appointment
Simplifying Surgery Experience
Consult with our expert surgeon for more than 50+ diseases
- Once you share your details, our care coordinator will get in touch with you.
- The coordinator will understand your symptoms and health condition in detail.
- Your consultation will be scheduled at the earliest.
Complications Possible with Balanitis
While balanitis itself does not usually interfere with physiological functions, if left untreated or chronic, it can lead to several serious complications:
-
Lichen Sclerosus
- Lichen sclerosus occurs when white, hard patches form on the skin. These patches can interfere with urination and the flow of semen through the urethra, potentially causing long-term discomfort and complications.
-
Scar Tissue
- Prolonged inflammation from balanitis can cause scarring around the head of the penis. This may result in a tight foreskin that is difficult or impossible to retract, leading to further irritation and difficulty with hygiene.
-
Ulcerative Lesions
- Balanitis can cause painful sores or ulcers that may bleed. Over time, these lesions can scar and further complicate the condition, making treatment more difficult.
-
Increased Risk of Cancer
- Chronic balanitis, especially if untreated, may increase the risk of developing penile cancer. Prompt and effective treatment can significantly reduce the chances of developing cancer related to this condition.
Risks Involved in Balanitis Surgery (Circumcision)
Circumcision is often performed to treat recurrent or severe cases of balanitis. While the procedure is generally safe, there are potential risks and complications associated with surgery:
-
Excessive Bleeding
- Some bleeding is expected during and after circumcision, but excessive or prolonged bleeding can occur, requiring medical intervention.
-
Infection
- Although infection rates after circumcision are low, they can still occur. Symptoms of infection include redness around the surgical site, swelling, pus, and fever. Prompt medical attention is necessary if these symptoms arise.
-
Foreskin Issues
- If the circumcision is not performed correctly, issues with the remaining foreskin can occur, such as:
- Paraphimosis: The foreskin becomes stuck behind the glans and cannot return to its normal position.
- Tight Frenulum: The band of tissue connecting the foreskin to the glans may become tight, leading to discomfort.
- Foreskin Infection: If the procedure leaves excess foreskin, it can lead to further infections or irritation.
- If the circumcision is not performed correctly, issues with the remaining foreskin can occur, such as:
-
Reattachment of Foreskin
- Improper healing or surgical technique could result in the foreskin reattaching incorrectly. This condition may require corrective surgery to prevent further discomfort and complications.
-
Wound Complications
- Rarely, the healing process may be delayed or complicated due to poor postoperative care or other factors, resulting in problematic scarring or skin issues.
-
Reaction to Anesthesia
- Though rare, some patients may experience adverse reactions to anesthesia, such as nausea or vomiting. These side effects typically subside after a few hours, but if they persist, medical attention is required.
-
Balanoposthitis
- This is inflammation of both the foreskin and glans, commonly affecting uncircumcised men. It can cause itching, swelling, and irritation, particularly in those with diabetes or phimosis.
Safe Surgical Options
For those considering circumcision for balanitis treatment, laser circumcision by an experienced urologist is generally recommended. This minimally invasive procedure has a lower risk of complications and a faster recovery time compared to other methods. Consulting with a skilled urologist ensures that the procedure is performed safely, minimizing risks and promoting a quick and smooth recovery
Make An Appointment
Simplifying Surgery Experience
Consult with our expert surgeon for more than 50+ diseases
- Once you share your details, our care coordinator will get in touch with you.
- The coordinator will understand your symptoms and health condition in detail.
- Your consultation will be scheduled at the earliest.
Non-Surgical Treatments for Balanitis
Before opting for surgery, your urologist may suggest non-surgical alternatives for treating balanitis, particularly in cases caused by fungal or bacterial infections. The treatment will depend on the underlying cause of your condition.
Antifungal Creams
If your balanitis is caused by a yeast infection (candida balanitis), antifungal creams are commonly prescribed. These creams should be applied to the head of the penis and foreskin. Some widely used antifungal treatments include:
- Lotrimin
- Cyclosporine ointment
- Gladic
- Glafine
- Mycophenolate
- Glazon
- 0.05% fluticasone propionate
- 2.0% sertaconazole nitrate
These medications help reduce inflammation and fight fungal infections, providing relief from balanitis symptoms.
Antibiotics
If your balanitis is caused by a bacterial infection, especially from a sexually transmitted disease (STD), antibiotics may be prescribed. Depending on the infection, the type of antibiotics will vary:
- Amoxicillin: Commonly prescribed for bacterial infections but may not be as effective for balanitis. Some brand names include Moxatag.
- Doxycycline: A tetracycline antibiotic used for severe cases of balanitis caused by STDs like chlamydia or gonorrhea. Brand names include Vibramycin and Sumycin.
- Ceftriaxone: Administered via injection, ceftriaxone is effective against gonorrhea and other bacterial infections. Some brand names include Cefixime and Ciprofloxacin.
It’s crucial to consult with a healthcare provider before using these medications to ensure they’re appropriate for your condition.
Home Remedies
While there are no proven home remedies for curing balanitis, some tips can help manage the symptoms and provide relief:
-
Use Mild Soaps: Opt for mild, unscented soaps to avoid further irritation. Scented soaps, bubble baths, and harsh chemicals can aggravate the condition.
-
Apply Coconut Oil: Coconut oil has soothing properties and can help with mild skin irritation. The lauric and caprylic acids in coconut oil are effective in calming irritated skin, providing relief for balanitis.
-
Yogurt: Rich in probiotics, yogurt helps promote the growth of beneficial bacteria in the body, which can fight infections. Applying yogurt directly to the affected area or consuming it regularly may reduce swelling and irritation.
-
Apple Cider Vinegar: Apple cider vinegar is known for its antifungal properties, particularly in cases of candida balanitis. Mix apple cider vinegar with water and apply it topically to the affected area to reduce swelling and combat the infection.
Always consult with a healthcare provider before starting any new treatment or home remedy to ensure it’s suitable for your condition.
Make An Appointment
Simplifying Surgery Experience
Consult with our expert surgeon for more than 50+ diseases
- Once you share your details, our care coordinator will get in touch with you.
- The coordinator will understand your symptoms and health condition in detail.
- Your consultation will be scheduled at the earliest.
Recurrent Balanitis & Why It Occurs
Recurrent balanitis refers to the repeated occurrence of inflammation of the glans (head of the penis) and foreskin. This condition can lead to significant discomfort and, if left unmanaged, can result in frequent flare-ups. Recurrent balanitis requires careful medical attention to manage symptoms and prevent future episodes.
Causes of Recurrent Balanitis:
-
Poor Hygiene: Inadequate cleaning can result in the accumulation of smegma (a combination of skin cells, oils, and moisture) under the foreskin, which can irritate the glans and foreskin, contributing to recurrent infections.
-
Infections: Bacterial and fungal infections, particularly Candida (yeast infections), are common causes. Sexually transmitted infections (STIs) like gonorrhea or chlamydia can also cause balanitis, leading to recurring episodes.
-
Irritants: Exposure to chemicals such as soaps, detergents, or spermicides can irritate the sensitive skin of the penis and foreskin, triggering balanitis.
-
Underlying Health Conditions: Conditions such as diabetes can predispose individuals to recurrent balanitis due to high blood sugar levels that encourage bacterial and fungal growth. Phimosis, a condition where the foreskin is too tight, can also contribute to recurring infections and inflammation.
-
Allergic Reactions: Allergies to latex condoms or certain lubricants can cause irritation and inflammation of the glans and foreskin.
-
Skin Conditions: Skin conditions like dermatitis and psoriasis can cause chronic inflammation of the glans, leading to recurrent balanitis episodes.
Preventing Recurrent Balanitis:
To prevent balanitis from becoming a recurrent issue, the following measures are recommended:
- Good Hygiene: Maintain regular and thorough hygiene practices, particularly under the foreskin, to prevent the buildup of smegma and irritants.
- Manage Chronic Conditions: Keep conditions like diabetes under control to reduce the risk of infections and inflammation.
- Avoid Irritants: Refrain from using harsh soaps, detergents, and irritants that could trigger inflammation.
- Regular Medical Check-Ups: Routine check-ups with a healthcare provider will help detect early signs of balanitis and manage symptoms effectively.
Sexual Activities & Balanitis
Balanitis itself is not a contagious condition, but the underlying infection causing it can be transmitted to a sexual partner. Therefore, it is important to avoid sexual activity until the infection has been treated and fully healed.
Before Treatment:
- Sexual Intercourse: If you have balanitis, your urologist will likely advise you to refrain from sexual activity. Engaging in intercourse may irritate the affected area and worsen symptoms.
- Masturbation: It is also recommended to avoid masturbation, as excessive friction may aggravate the condition and delay healing.
After Treatment:
- Post-Circumcision: If circumcision is performed as part of the treatment for balanitis, it is advisable to avoid sexual activity for at least 3-4 weeks to allow the wound to heal properly.
- Resuming Sexual Activity: Once the circumcision wound has healed and your urologist has cleared you for sexual activity, you can resume normal sexual activity with your partner.
- Masturbation: After healing, you can also return to masturbation, as long as your urologist deems it safe.
By following these recommendations and maintaining proper care, recurrent balanitis can be managed effectively, reducing the chances of further flare-ups.
Make An Appointment
Simplifying Surgery Experience
Consult with our expert surgeon for more than 50+ diseases
- Once you share your details, our care coordinator will get in touch with you.
- The coordinator will understand your symptoms and health condition in detail.
- Your consultation will be scheduled at the earliest.
Complications with Untreated Balanitis
While balanitis often progresses slowly and may not immediately interfere with physiological functions, leaving it untreated can result in several serious complications over time. These include:
-
Lichen Sclerosus:
Lichen sclerosus is a chronic inflammatory skin condition that can affect the skin of the genitals. It may cause thinning, white patches on the skin, and in some cases, it can interfere with urination and the passage of semen through the urethra. If untreated, lichen sclerosus can cause permanent skin damage. -
Scar Tissue Formation:
Chronic or untreated balanitis can lead to the formation of scar tissue on the penis, particularly around the head (glans). This can cause the foreskin to become tight, resulting in conditions like phimosis (a tight foreskin that cannot be retracted) or paraphimosis (where the foreskin is stuck behind the head of the penis and cannot be moved back over it), both of which can cause further discomfort and complications. -
Ulcerative Lesions:
Prolonged balanitis can lead to the development of painful ulcerative lesions or sores on the penis. These lesions can bleed and become infected, leading to additional complications such as scarring or further infection. -
Increased Risk of Penile Cancer:
Although rare, chronic balanitis can significantly increase the risk of developing penile cancer. In particular, if balanitis is left untreated and leads to long-term inflammation, it can increase the likelihood of developing cancer in the affected area.
Why Timely Treatment is Important
If you’re experiencing symptoms of balanitis, such as redness, irritation, swelling, or discharge, it is crucial to seek medical attention early. Early diagnosis and treatment can prevent these complications and help manage symptoms effectively.
Types of Infections in the Penis
Penile infections can arise from various pathogens, including bacteria, fungi, and viruses. These infections can present with different symptoms and require different treatments. Here are some common types of penile infections:
-
Balanitis:
Balanitis is the inflammation of the glans (head) of the penis, often caused by poor hygiene, irritants, or infections by bacteria or yeast. Symptoms include redness, swelling, pain, and discharge from the penis. Treatment involves practicing proper hygiene and, depending on the cause, using antifungal or antibiotic medications. -
Phimosis:
Phimosis occurs when the foreskin cannot be fully retracted over the glans, which can cause discomfort, difficulty urinating, and increase the risk of infections. This condition is often treated with topical steroid creams to help loosen the foreskin. In severe cases, circumcision may be necessary. -
Paraphimosis:
Paraphimosis is when the retracted foreskin cannot be returned to its normal position over the glans, leading to swelling and restricted blood flow. It is considered a medical emergency, as it can cause permanent tissue damage if not treated promptly. Treatment often involves manual reduction of the foreskin, though in severe cases, surgical intervention may be required. -
Yeast Infections:
Yeast infections are caused by the fungus Candida and are more common in men who are uncircumcised. Symptoms include itching, redness, rashes, and sometimes thick, white discharge. Antifungal creams or oral medications are typically prescribed for treatment. -
Chlamydia:
Chlamydia is a common sexually transmitted infection (STI) that may not show symptoms initially, but it can cause burning during urination, discharge, and testicular pain. Chlamydia is treated with antibiotics, and it is important to complete the prescribed course to fully eradicate the infection. -
Gonorrhea:
Gonorrhea is another STI that presents symptoms like a burning sensation during urination, pus-like discharge from the penis, and swelling. It is treated with antibiotics, and timely treatment is necessary to avoid complications. -
Bacterial Infections:
Bacterial infections, such as cellulitis, can affect the penile skin, often due to skin injuries or poor hygiene. Symptoms include redness, warmth, swelling, and pain at the site of infection. Antibiotic treatment is required to clear bacterial infections.
Prevention and Management
To prevent penile infections, it is important to:
- Maintain good hygiene by regularly cleaning the penis, especially under the foreskin (if uncircumcised).
- Practice safe sex by using condoms to prevent the transmission of STIs.
- Seek prompt medical attention for any unusual symptoms, such as itching, pain, discharge, or swelling.
Early treatment and proper care can help prevent complications and ensure better outcomes.