Make An Appointment
Simplifying Surgery Experience
Consult with our expert surgeon for more than 50+ diseases
- Once you share your details, our care coordinator will get in touch with you.
- The coordinator will understand your symptoms and health condition in detail.
- Your consultation will be scheduled at the earliest.
Phimosis Treatment - Laser Surgery- Procedure & Benefits at Curific Health Care
Get In Touch
Make an Appointment
What is Phimosis?
Phimosis is a medical condition where the foreskin, the retractable skin covering the head of the penis (glans), cannot be pulled back or retracted.
While phimosis is often harmless and does not necessarily require treatment, it can cause discomfort, pain, or complications such as infections or difficulty urinating in severe cases. When these symptoms occur, surgical treatments like circumcision or partial removal of the foreskin may be recommended.
Phimosis is a natural occurrence in most newborns and young boys, as the foreskin remains attached to the glans. Typically, this resolves on its own as the foreskin loosens with age, usually by adolescence. However, in some individuals, phimosis may persist into adulthood.
Non-surgical treatments, such as applying steroid creams, can provide temporary relief and may help in some cases. For adults with recurring or severe symptoms, surgical procedures are considered a safe and effective solution to address phimosis.
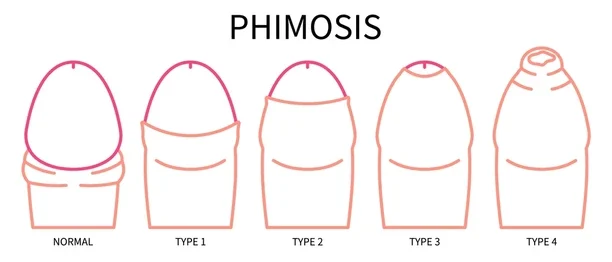
What Are the Types of Phimosis?
Phimosis can be categorized into two types: physiological phimosis and pathological phimosis.
Physiological Phimosis:
This type, also known as primary phimosis, is a natural condition present at birth. In almost all newborns, the foreskin remains tight and adheres to the glans of the penis. Over time, the foreskin naturally loosens and becomes retractable as the child grows. This process typically resolves on its own by adolescence.
- Treatment is often unnecessary for physiological phimosis, but if the foreskin remains tight into teenage years, non-surgical options like steroid creams may be recommended. In persistent cases, surgical procedures like circumcision may be required.
Pathological Phimosis:
Also referred to as secondary phimosis, this condition results from scarring, infection, or inflammation due to an injury, poor hygiene, or forced retraction of the foreskin. Pathological phimosis can occur at any age and often requires medical attention or surgical intervention.
Common causes of pathological phimosis include:
- Poor hygiene practices
- Chronic infections like balanitis (inflammation of the glans) or balanoposthitis (inflammation of the glans and foreskin)
- Skin conditions, such as lichen sclerosus
- Scar tissue formation from trauma or repeated infections
Both types require evaluation by a healthcare provider to determine the most appropriate course of treatment based on severity and symptoms.
Get In Touch
Make an Appointment
Make An Appointment
Simplifying Surgery Experience
Consult with our expert surgeon for more than 50+ diseases
- Once you share your details, our care coordinator will get in touch with you.
- The coordinator will understand your symptoms and health condition in detail.
- Your consultation will be scheduled at the earliest.
Diagnosis for Phimosis
Before proceeding with surgery, your healthcare provider will perform a series of evaluations to assess your condition and rule out any underlying health complications.
Physical Examination:
The diagnostic process usually begins with a physical examination. The doctor will attempt to gently retract the foreskin over the glans. If the foreskin cannot be retracted or the glans is not fully visible, phimosis is confirmed.
Medical History and Symptoms:
Your urologist may ask about:
- Past medical or surgical history
- Symptoms like pain, discomfort, or difficulty in urination
- Any penile injuries
- Sexual activity and related concerns
Infection and Injury Assessment:
The doctor may check for redness, swelling, or discharge to identify signs of infection or trauma that could be contributing to the condition.
Non-Surgical Options:
In mild cases, non-surgical treatments such as steroid creams may be tried first. If these fail to provide relief, surgical intervention will be recommended.
Surgical Treatment for Phimosis – Circumcision
Circumcision is a commonly performed surgical treatment for phimosis. The procedure involves the removal of the foreskin and can be performed using various techniques:
Laser Circumcision:
- A minimally invasive procedure using a focused laser beam to remove the foreskin precisely.
- The high temperature of the laser also seals blood vessels, reducing bleeding.
- Provides quicker recovery and minimal risk of infection.
Stapler Circumcision:
- Performed using a specialized disposable stapler device designed for circumcision.
- The device removes the foreskin in one motion and places a silicone ring around the wound to minimize bleeding.
- The silicone ring falls off naturally within 7-10 days as the wound heals.
Open Circumcision (Dorsal Slit Technique):
- A traditional method where the foreskin is cut using a scalpel or surgical scissors.
- More invasive compared to laser or stapler methods, requiring a longer recovery period.
- Carries a higher risk of infection and complications due to the nature of the procedure.
Each surgical method is chosen based on the patient’s condition, preferences, and the doctor’s recommendation.
Make An Appointment
Simplifying Surgery Experience
Consult with our expert surgeon for more than 50+ diseases
- Once you share your details, our care coordinator will get in touch with you.
- The coordinator will understand your symptoms and health condition in detail.
- Your consultation will be scheduled at the earliest.
Why Choose Circumcision for Phimosis?
Before recommending circumcision, your urologist may explore non-surgical treatments like steroid creams or ointments for phimosis. However, circumcision is widely regarded as the most reliable and long-term solution for phimosis.
Effectiveness:
While phimosis ointments may provide temporary relief, the condition often recurs after discontinuing the medication. Circumcision permanently removes the foreskin, eliminating the risk of phimosis returning.
Additional Benefits:
- Improved genital hygiene, making cleaning easier.
- Reduced risk of penile conditions like paraphimosis or balanitis.
- Prevention of potential infections and inflammation in the future.
Recovery After Circumcision
Recovery typically takes about 7-10 days, but this may vary based on factors like the surgical technique, your overall health, and postoperative care quality. Adhering to your doctor’s instructions is essential for a smooth recovery.
Postoperative Guidelines:
- Keep the surgical site dry for the first 48 hours.
- Avoid smoking or alcohol consumption to promote healing.
- Stay hydrated by drinking 7-8 glasses of water daily.
- Refrain from swimming or using public baths.
- Avoid sexual intercourse until cleared by your doctor.
- Limit strenuous physical activities that could strain the penis or surrounding areas.
Make An Appointment
Simplifying Surgery Experience
Consult with our expert surgeon for more than 50+ diseases
- Once you share your details, our care coordinator will get in touch with you.
- The coordinator will understand your symptoms and health condition in detail.
- Your consultation will be scheduled at the earliest.
Benefits of Phimosis Surgery
Phimosis surgery, primarily through circumcision, not only resolves the condition but also offers several health benefits:
- Enhanced Hygiene: The removal of the foreskin makes it easier to maintain cleanliness by eliminating the accumulation of smegma and bacteria around the glans.
- Reduced UTI Risk: Circumcision lowers the likelihood of urinary tract infections by preventing bacterial buildup.
- Lower Risk of STDs: While not a substitute for safe practices, circumcised men are at a slightly reduced risk of contracting sexually transmitted diseases.
- Prevention of Penile Cancer: Though rare, the risk of penile cancer is significantly lower in circumcised men.
- Eliminates Foreskin-related Issues: Conditions like balanitis, phimosis, and paraphimosis are effectively treated or prevented.
- Improved Sexual Health: By addressing phimosis, patients can experience less pain and improved sexual function.
How to Prepare for Phimosis Surgery
While circumcision requires minimal preparation, following these simple steps will ensure a smooth process:
- Fasting: Avoid eating for at least 6 hours before surgery, but stay hydrated by drinking water as advised.
- Pre-surgical Hygiene: Take a bath or shower and clean the genital area thoroughly. Shave any pubic hair if recommended.
- Wear Supportive Clothing: Opt for snug briefs to support the penis post-surgery and hold the dressing in place.
- Transport Arrangement: Arrange for someone to drive you home or accompany you in a cab post-surgery.
- Avoid Smoking and Alcohol: Refrain from smoking or consuming alcohol for at least 48 hours before the procedure.
- Medication Disclosure: Inform your doctor about any medications you are taking, as some may need to be paused temporarily.
- Plan Time Off: Ensure you take a few days off work for rest and recovery.
Make An Appointment
Simplifying Surgery Experience
Consult with our expert surgeon for more than 50+ diseases
- Once you share your details, our care coordinator will get in touch with you.
- The coordinator will understand your symptoms and health condition in detail.
- Your consultation will be scheduled at the earliest.
Non-Surgical Treatment for Phimosis
Medications
For treating phimosis caused by infections or skin conditions, your doctor may prescribe medications. Always consult your healthcare provider before starting any medication. Some commonly prescribed medications include:
- Antibiotics or antifungal creams like Lotrimin.
- Cyclosporine ointment for inflammation.
- Methotrexate for certain skin conditions.
- Prednisone (a corticosteroid) for reducing swelling.
- Mycophenolate for severe autoimmune reactions.
- Antibiotics like Azithromycin and Doxycycline for bacterial infections.
Home Remedies
Non-invasive techniques for managing mild to moderate cases of phimosis include:
- Foreskin Stretching: Gradual stretching of the foreskin under your doctor’s guidance can improve elasticity and reduce tightness.
- Ointments: Use doctor-recommended steroid-based ointments to relieve pain, inflammation, or infections.
- Retracting Exercises: Gentle retraction of the foreskin over the glans daily can help improve mobility. Avoid forceful attempts to stretch the foreskin.
- Proper Hygiene: Regular cleaning with mild soap can prevent bacterial or smegma buildup and reduce risks of infection.
- Coconut Oil: Using coconut oil during stretching exercises can ease the process and reduce discomfort.
Best Way to Cure Phimosis
Laser circumcision is widely regarded as the safest and most effective treatment. It uses a precise laser beam to remove the excess foreskin without causing deep cuts or excessive bleeding. Benefits include:
- Faster recovery compared to conventional methods.
- Minimal risk of complications.
- Improved post-surgery quality of life.
Phimosis in Adulthood
While phimosis naturally resolves in most children, some cases persist into adulthood, requiring treatment. Adult phimosis can cause complications like pain, infections, or issues during sexual activity. If untreated, it might necessitate more complex surgeries. Consult a urologist if you notice persistent symptoms to prevent further health risks and ensure proper management.
Make An Appointment
Simplifying Surgery Experience
Consult with our expert surgeon for more than 50+ diseases
- Once you share your details, our care coordinator will get in touch with you.
- The coordinator will understand your symptoms and health condition in detail.
- Your consultation will be scheduled at the earliest.
Side Effects of Phimosis Surgery
After undergoing circumcision for phimosis, minor side effects such as mild swelling, slight bleeding, and discomfort are common and expected. These effects usually resolve within a few days without requiring additional treatment.
However, if these side effects persist or worsen, it could indicate complications that need medical attention. Contact your healthcare provider promptly if symptoms do not improve.
Some possible complications include:
- Excessive bleeding around the surgical area.
- Infections near the incision site.
- Formation of scar tissue that could affect healing.
- Tenderness or sensitivity around the scar.
- Reduced sensation in the penile glans (head of the penis).
- Adverse reactions to anesthesia.
What if Phimosis is Left Untreated?
Phimosis without symptoms does not necessarily require treatment. However, if left untreated when symptoms like pain, difficulty urinating, or ballooning of the foreskin are present, it can lead to severe complications, including:
- Recurrent infections such as balanitis or UTIs.
- Gangrene in extreme cases of infection.
- Increased risk of penile cancer.
- Permanent damage to the penile tissue.
- In severe cases, partial or complete loss of the penis.
Phimosis vs. Paraphimosis
While phimosis and paraphimosis are conditions affecting the foreskin of the penis, they are distinct in their causes, symptoms, and treatments. Below is a comparison highlighting their key differences:
| Aspect | Phimosis | Paraphimosis |
|---|---|---|
| Definition | Inability to retract the foreskin over the penile glans (head of the penis). | Foreskin becomes trapped behind the penile glans after being retracted and cannot return to its normal position. |
| Severity | Usually not a medical emergency. | Considered a urological emergency. |
| Common Symptoms | – Swelling- Tenderness- Blood in urine- Weak urine stream- Pain with erection or sexual activity | – Pain- Swelling- Discoloration of the penis- Inability to pull the foreskin back over the head of the penis |
| Causes | Often occurs naturally, due to infections, inflammation, poor hygiene, or scar tissue. | Usually caused by improper handling during catheterization, medical procedures, or forceful retraction. |
| Treatment | – Medications like corticosteroid creams- In severe cases, circumcision or preputioplasty | – Circumcision or manual reduction of the foreskin- Emergency intervention to restore blood flow |
| Complications | If untreated, it can lead to infections, gangrene, swelling, or in extreme cases, loss of the penis. | If untreated, it can result in ischemia (tissue damage) or necrosis (tissue death). |
Key Takeaway:
- Phimosis generally progresses slowly and can often be managed with non-surgical treatments, although severe cases might require circumcision.
- Paraphimosis requires immediate medical intervention to prevent serious complications such as tissue death.
Make An Appointment
Simplifying Surgery Experience
Consult with our expert surgeon for more than 50+ diseases
- Once you share your details, our care coordinator will get in touch with you.
- The coordinator will understand your symptoms and health condition in detail.
- Your consultation will be scheduled at the earliest.
Ointments & Creams for Phimosis
Various steroid-based and non-steroid-based ointments are commonly used to treat phimosis. These ointments work by softening and loosening the foreskin, offering a success rate of approximately 70%. Below are some widely used options:
Betnovate-N
- Active Ingredient: Betamethasone valerate (steroid) + Neomycin sulfate (antibacterial).
- Effectiveness: Helps with conditions like eczema, psoriasis, and lichen planus, often linked to phimosis. Reduces redness, swelling, and irritation.
- Usage: Apply 2-3 times daily for 4-6 weeks. Not recommended for children under 1 year.
Temovate
- Active Ingredient: Clobetasol propionate (0.05%).
- Effectiveness: Treats eczema, psoriasis, and other skin conditions associated with phimosis. Reduces swelling, itching, and redness.
- Usage: Use twice daily for no more than two weeks to avoid side effects.
Canesten
- Active Ingredient: Clotrimazole (anti-fungal).
- Effectiveness: Prescribed when phimosis is caused by fungal infections. Reduces inflammation and soreness.
Elocon
- Active Ingredient: Mometasone furoate (0.1%).
- Effectiveness: Treats inflammation from conditions like eczema, lichen planus, and psoriasis. Available as an ointment, cream, or lotion.
- Usage: Effective within 2 weeks. Not recommended for children under 2 years.
Novoglan
- Active Ingredients: Natural oils (neem, jojoba, primrose), rose geranium, rice bran, and Vitamin E.
- Effectiveness: Softens and stretches the foreskin with anti-inflammatory and antioxidant properties.
- Usage: Apply daily before foreskin stretching exercises.
Aristospan
- Active Ingredient: Triamcinolone acetonide.
- Effectiveness: Reduces pain and soreness, aiding in loosening and retracting the foreskin when combined with stretching exercises.
Hydrocortisone
- Active Ingredient: Hydrocortisone (mild corticosteroid).
- Effectiveness: Reduces inflammation and itching, particularly useful for phimosis linked to eczema and psoriasis. Often combined with antimicrobial agents to treat infections.
Ilotycin
- Active Ingredient: Erythromycin (antibiotic).
- Effectiveness: Treats bacterial infections that may cause or worsen phimosis.
Key Considerations
- Always consult a healthcare professional before starting treatment.
- Use as directed to avoid potential side effects, such as skin thinning or irritation.
- While these creams can provide relief, severe cases of phimosis might require surgical intervention.