Make An Appointment
Simplifying Surgery Experience
Consult with our expert surgeon for more than 50+ diseases
- Once you share your details, our care coordinator will get in touch with you.
- The coordinator will understand your symptoms and health condition in detail.
- Your consultation will be scheduled at the earliest.
Uterine Fibroids - Treatment Procedure & Benefits at Curific Health Care
Get In Touch
Make an Appointment
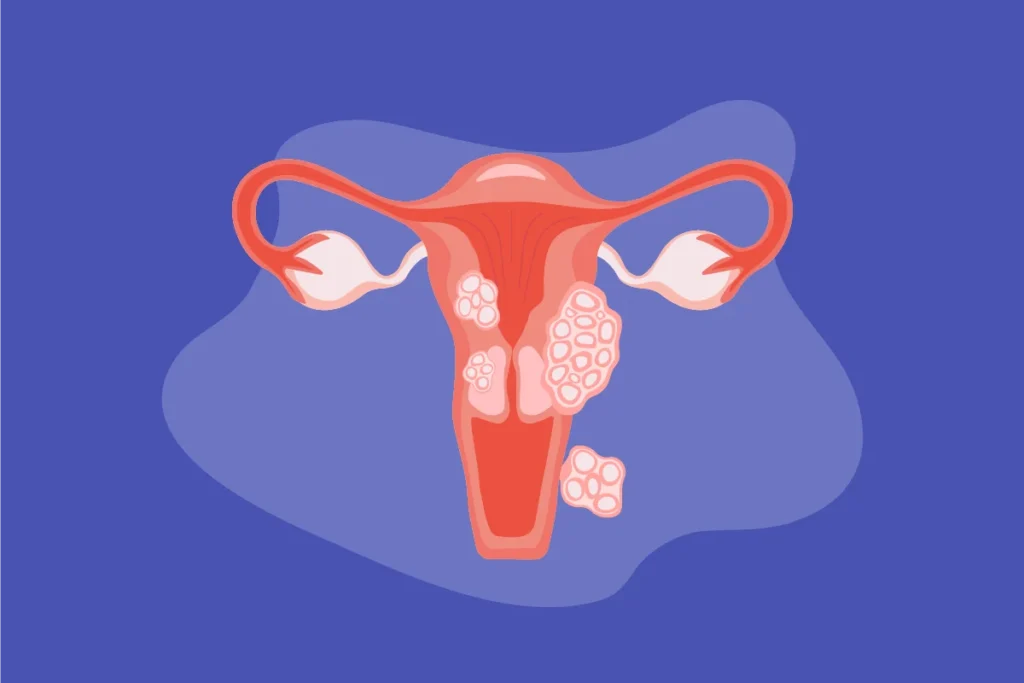
What is Uterine Fibroids?
Uterine fibroids, also known as Rasoli in Hindi, are the most common non-cancerous tumors of the uterus. These growths typically develop during the childbearing years and vary in size, shape, and location. Fibroids can be found within the uterus, embedded in the uterine wall, or on its outer surface.
In most cases, uterine fibroids are painless and do not cause noticeable symptoms. However, when symptoms occur, they may include heavy periods, pelvic pain, or difficulty conceiving.
Treatment options for uterine fibroids include:
- Medications: Used to manage symptoms and reduce fibroid size.
- Surgical Treatment: Recommended for severe cases, larger fibroids, or multiple growths.
The choice of treatment depends on factors such as the size, number, and severity of the fibroids. Consulting a gynecologist is essential for an accurate diagnosis and effective management.
Make An Appointment
Simplifying Surgery Experience
Consult with our expert surgeon for more than 50+ diseases
- Once you share your details, our care coordinator will get in touch with you.
- The coordinator will understand your symptoms and health condition in detail.
- Your consultation will be scheduled at the earliest.
Which size of fibroid is dangerous?
Fibroids larger than 4 cm can pose significant health risks. Here’s why:
- Obstruction of Fallopian Tubes: Fibroids that develop within the uterine muscles may swell and block the fallopian tubes, affecting fertility and causing complications.
- Pressure on Surrounding Organs: If fibroids grow outside the uterus, they can press on nearby structures, including the pleura (lining of the chest), leading to discomfort or pain.
- Risk of Rupture: Large fibroids may outgrow their blood supply, causing tissue death (degeneration) and potential rupture, leading to severe pain and medical emergencies.
- Pregnancy Complications: Fibroids of significant size can interfere with implantation, increase the risk of miscarriage, or lead to other complications during pregnancy.
It’s crucial to monitor fibroids with regular medical checkups and consult a gynecologist for appropriate treatment if they grow large or cause symptoms.
Get In Touch
Make an Appointment
Make An Appointment
Simplifying Surgery Experience
Consult with our expert surgeon for more than 50+ diseases
- Once you share your details, our care coordinator will get in touch with you.
- The coordinator will understand your symptoms and health condition in detail.
- Your consultation will be scheduled at the earliest.
Diagnostic Tests for Uterine Fibroids
To accurately diagnose uterine fibroids, the doctor evaluates the patient’s medical history and performs a physical examination. Based on the severity, size, and location of fibroids, the following diagnostic tests may be recommended:
Pelvic Ultrasound:
- Uses high-frequency sound waves to produce images of the uterus and fibroids.
- Helps locate and determine the size of fibroids.
Abdominal and Pelvic CT Scan:
- Offers detailed images of soft tissues, blood vessels, and internal organs, helping to assess the condition more precisely.
Pelvic MRI Scan:
- Provides detailed images of the uterus and surrounding structures using a magnetic field, making it easier to evaluate fibroid size and location.
Blood Tests:
- Includes a Complete Blood Count (CBC) to check for anemia due to heavy bleeding.
- Hormonal tests to measure estrogen and progesterone levels.
Hysteroscopy:
- A probe is inserted through the cervix to examine the uterus cavity, especially useful for detecting submucosal fibroids.
Hysterosalpingography (HSG):
- Used to evaluate the structure of the uterus and fallopian tubes, particularly for individuals facing infertility.
- A dye is injected, and X-rays are taken to study the reproductive organs.
Tumor Biopsy:
- Involves extracting a tissue sample from the fibroid for microscopic examination to confirm the diagnosis.
Treatment Procedure for Uterine Fibroids
Treatment options depend on factors like the severity of symptoms, fibroid size and location, patient’s age, pregnancy status, and plans for future pregnancies.
1. Medical Treatment for Uterine Fibroids
Medications are primarily used to manage symptoms or shrink fibroids but do not eliminate them completely:
Gonadotropin-Releasing Hormone (GnRH) Agonists:
- Suppress the production of estrogen and progesterone, inducing temporary menopause.
- Reduce fibroid size and improve symptoms like heavy bleeding.
- Limited use (3–6 months) due to side effects like bone loss.
Tranexamic Acid:
- Helps control heavy menstrual bleeding but does not shrink fibroids.
- Taken only during heavy bleeding days.
Nonsteroidal Anti-inflammatory Drugs (NSAIDs):
- Relieve pain but do not affect fibroid size or bleeding.
2. Surgical Treatment for Uterine Fibroids
Surgery is recommended for large or symptomatic fibroids, and the options include:
Myomectomy:
- Removes fibroids while preserving the uterus, ideal for women who wish to have children.
- Can be performed through open surgery, laparoscopy, or hysteroscopy.
Hysterectomy:
- Complete removal of the uterus, recommended for severe cases where fibroids cause significant symptoms.
- A definitive solution, but it eliminates the possibility of future pregnancies.
Uterine Artery Embolization (UAE):
- Minimally invasive procedure where blood flow to the fibroids is blocked, causing them to shrink.
Endometrial Ablation:
- Destroys the lining of the uterus to control bleeding but is not suitable for women planning future pregnancies.
Radiofrequency Ablation (RFA):
- Uses heat to destroy fibroids while preserving healthy uterine tissue.
Choosing the Right Option
The decision between medical and surgical treatment depends on the patient’s symptoms, medical history, and reproductive goals. Consulting with a gynecologist ensures a personalized treatment plan for optimal outcomes.
Make An Appointment
Simplifying Surgery Experience
Consult with our expert surgeon for more than 50+ diseases
- Once you share your details, our care coordinator will get in touch with you.
- The coordinator will understand your symptoms and health condition in detail.
- Your consultation will be scheduled at the earliest.
Surgical Treatment Options for Uterine Fibroids
1. Radio-Frequency Ablation (RFA)
- A minimally invasive procedure that uses heat to shrink fibroids and the blood vessels supplying them.
- Recommended for:
- Patients with smaller fibroids.
- Uterus below the navel.
- No history of complex abdominal surgeries.
- Benefits:
- Reduces fibroid size significantly.
- Limitations:
- Fibroids may not be completely eliminated.
- New fibroids can develop, and existing ones might regrow.
2. Hysteroscopic Myomectomy
- Designed to remove submucosal fibroids within the uterine cavity.
- Procedure:
- A hysteroscopic resectoscope is inserted through the vagina and cervix to access and remove fibroids using an electrosurgical wire loop.
- Ideal for women looking to preserve their uterus and address symptoms like abnormal bleeding or infertility caused by submucosal fibroids.
3. Endometrial Ablation
- Targets fibroids causing heavy or abnormal bleeding.
- Procedure:
- Instruments using heat, microwave energy, hot water, or electric currents are inserted into the uterus to destroy its lining.
- Not suitable for:
- Pregnant women or those planning future pregnancies.
- Benefit:
- Reduces bleeding and fibroid-related symptoms.
4. Myolysis and Cryomyolysis
- Treats fibroids located near the uterine surface.
- Procedure:
- Small incisions are made to insert surgical devices that direct heat (electrical current or laser) or cold energy to cut off the blood supply to fibroids.
- Outcome:
- Fibroids shrink over time without surgical removal.
- Note:
- This approach is less invasive but may not be suitable for very large fibroids.
5. MRI-Guided Focused Ultrasound Surgery (FUS)
- A non-invasive procedure performed within an MRI scanner.
- Procedure:
- The doctor uses MRI imaging to locate fibroids precisely.
- Focused ultrasound waves are directed at fibroids to heat and destroy them.
- Benefits:
- Preserves the uterus.
- No surgical incisions required.
- Suitable for:
- Women with fewer and well-defined fibroids.
These procedures offer various solutions for managing fibroids, allowing patients and doctors to choose based on individual health conditions, severity of symptoms, and reproductive goals. Regular follow-ups post-procedure are essential to monitor fibroid status and prevent recurrence.
Who Gets Uterine Fibroids?
- Uterine Fibroids may affect females of any age but are mostly present in the 30-50 years age category (young and middle-aged adults are affected the most)
- These tumors are very common, about 70-80% of women usually have fibroids by the time they are 50 years old.
- Women with the rare genetic disorder, namely hereditary leiomyomatosis and renal cancer syndrome, may present with leiomyomas at an earlier age (while they are much younger)
- Africans and African Americans have a higher incidence of these tumors when compared to individuals of other racial groups or ethnicities (3:1 incident rate over other races/ethnic groups). In such individuals, the tumors are often seen to arise at a much younger age.
What are the Risk Factors for Uterine Fibroid?
The risk factors for uterine fibroids may include the following:
- Family history of the condition
- Imbalance of estrogen and progesterone hormone levels in the body
- Women of African descent are at a higher risk in comparison to individuals of other races/ethnic groups. In general, such women have larger fibroids, more signs and symptoms, and the tumors are known to grow more rapidly in size
- Early onset of menstruation (in girls)
- Obesity, being overweight
- A diet that’s high in meat and low in vegetables
- Vitamin D deficiency
- Excessive alcohol consumption
- Some variants are more common during the active reproductive phase (age) of a woman than others.
Make An Appointment
Simplifying Surgery Experience
Consult with our expert surgeon for more than 50+ diseases
- Once you share your details, our care coordinator will get in touch with you.
- The coordinator will understand your symptoms and health condition in detail.
- Your consultation will be scheduled at the earliest.
Who Gets Uterine Fibroids?
Uterine fibroids can affect women of any age but are most common among women aged 30-50.
- Prevalence:
- Approximately 70-80% of women develop fibroids by the age of 50.
- Genetic Predisposition:
- Women with hereditary leiomyomatosis and renal cancer syndrome are more likely to develop fibroids at a younger age.
- Ethnic Variations:
- African and African American women are 3 times more likely to develop fibroids compared to other racial groups.
- Fibroids in these populations often arise earlier, grow larger, and cause more symptoms.
Risk Factors for Uterine Fibroids
Genetics
- Family history of uterine fibroids significantly increases the risk.
Hormonal Imbalance
- High levels of estrogen and progesterone contribute to fibroid development and growth.
Race and Ethnicity
- Women of African descent are at higher risk, experiencing larger and faster-growing fibroids with more severe symptoms.
Early Menstruation
- Girls who begin menstruating at an early age are at greater risk.
Obesity
- Being overweight increases the likelihood of fibroids.
Dietary Habits
- A diet high in red meat and low in vegetables raises the risk.
Vitamin D Deficiency
- Low levels of vitamin D have been linked to fibroid growth.
Alcohol Consumption
- Excessive alcohol intake can contribute to the development of fibroids.
Reproductive Age
- Certain fibroid types are more prevalent during the active reproductive years of a woman.
Understanding these risk factors and prevalence can help in early detection, monitoring, and management of uterine fibroids.
Make An Appointment
Simplifying Surgery Experience
Consult with our expert surgeon for more than 50+ diseases
- Once you share your details, our care coordinator will get in touch with you.
- The coordinator will understand your symptoms and health condition in detail.
- Your consultation will be scheduled at the earliest.
How Can Uterine Fibroids Be Prevented?
There is no guaranteed way to prevent uterine fibroids. However, the following measures may help reduce the risk:
Maintain a Healthy Weight
- Adopt a balanced diet and engage in regular physical activity to manage weight, especially if you are overweight or obese.
Limit Alcohol Intake
- Avoid or minimize alcohol consumption to lower the risk of fibroid development.
Follow a Balanced Diet
- Incorporate more vegetables, fruits, and whole grains into your diet while reducing red meat consumption. A nutritious diet can also prevent mineral and vitamin deficiencies.
Attend Regular Prenatal Checkups
- For expectant mothers, consistent prenatal care helps monitor both maternal and fetal health.
Schedule Regular Medical Screenings
- Periodic blood tests, imaging scans, and physical examinations are crucial to detect and monitor fibroids, as there is a risk of recurrence.
Although these measures cannot guarantee prevention, they can contribute to overall health and potentially reduce the likelihood of fibroids developing or worsening.